Prostatitis is a disease characterized by the presence of inflammation and / or infection localized to the prostate.
May present with a wide range of clinical signs and complaints.
Anatomy
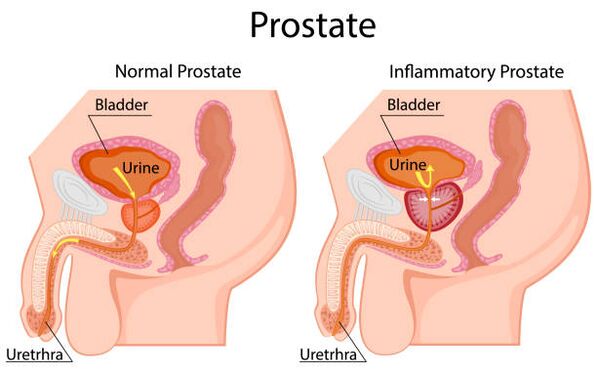
The prostate is a small gland that is part of the male reproductive system and a hormone-dependent organ. Its shape and size has been compared to a large walnut. A normal prostate weighs approximately 20 g, has a volume of 15 to 25 ml, and is 3 cm in length, 4 cm in width and 2 cm in depth.
The prostate is located in the small pelvis, below the bladder and above the rectum. The urethra, the urethra, passes through the thickness of the gland. The prostate is surrounded by a capsule made up of smooth muscles, collagen and elastic fibers; covered with three layers of dense connective tissue (fascia) on the anterior, lateral and posterior surfaces. The posterior aspect of the prostate is bordered by the bulb of the rectum. They are separated by the retrovesical fascia or Denonville fascia, which allows palpation of the posterior aspect of the prostate.
The prostate is made up of approximately 70% glandular tissue and 30% fibromuscular stroma. It is customary to divide the organ into 3 zones.
Transition zone.The transition zone accounts for 10% of glandular tissue and 20% of cases of malignant prostate tumors. In this area, one of the main age-related diseases in men is formed - benign prostatic hyperplasia, which can lead to difficulty urinating due to tissue overgrowth.
Central area.The area surrounding the ejaculatory ducts. Consists of glandular tissue, connective tissue and muscle elements. Tumors in this area are extremely rare.
Peripheral zone.Covers the posterior and lateral sides of the prostate and contains 70% of the glandular tissue. It is an area that is palpable across the rectum and allows the urologist to assess the condition of the prostate. Up to 70% of malignant tumors are localized precisely in the peripheral area. Therefore, digital rectal examination is an important diagnostic method and should be performed in patients over 45 years of age.
Functions of the prostate:
- production of prostatic secretion, which is an integral part of semen and takes part in the liquefaction of the ejaculate, as well as its saturation with nutrients such as various enzymes and vitamins, citric acid, zinc ions, which help improve motility and lsperm activity;
- The prostate contains smooth muscle fibers that help release sperm from the urethra during ejaculation, prevent sperm from entering the bladder, and participate in the urinary retention mechanism.
Prostatitis, benign prostatic hyperplasia and prostate cancer are the three main prostate diseases.
All three diseases can coexist in the same prostate at the same time. That is, the presence of prostatitis does not exclude the presence of prostatic hyperplasia and prostate cancer in the patient and vice versa.
Causes of prostatitis
According to statistics, prostatitis is the most common urological disease - after prostatic hyperplasia and prostate cancer - in men under 50 and the third most common in men over 50.
Prostatitis represents 6 to 8% of outpatient urological consultations.
The most common causative agent of prostatitis is the strain E. coli, which is detected in 80% of cases. Rarer pathogens are enterococci, Pseudomonas aeruginosa, Klebsiella and other gram-negative bacteria. The role of sexually transmitted infections (such as Chlamydia trachomatis) in prostate inflammation is not yet clearly established and is under investigation. In patients with HIV infection and other serious changes in the immune system, possible causative agents are cytomegalovirus, mycobacterium tuberculosis, fungi and other rare pathogens. There are data indicating the presence of microorganisms in the prostate that are not detected in standard studies, but play a role in the appearance of inflammatory changes and the subsequent development of symptoms of prostatitis.
The possible causes of prostatitis are:
- intraprostatic reflux of urine as a result of dysfunctional urination (urine, with certain predisposing factors, can enter the prostate through the ducts of the prostate, causing an inflammatory process);
- unprotected anal sex;
- narrowing of the foreskin (phimosis);
- autoimmune diseases;
- functional and anatomical changes in the muscles of the pelvic floor;
- changes in the central nervous system, including functional and anatomical changes in the brain;
- traumatic and unusual sexual activity;
- psychological factors (in a number of studies the influence of psychological stress on the appearance of symptoms of chronic prostatitis has been proven - in some patients psychosomatic disorders were diagnosed, in the treatment of which a decrease in symptomsof prostatitis and the likelihood of its relapse were noted).
Risk factors for prostatitis also include: abstinence or excessive sexual activity, habit of restricting ejaculation, smoking, night work, sedentary lifestyle, insufficient fluid intake, and poor diet.
Symptoms
- pain or burning sensation when passing urine (dysuria);
- urinary disorders;
- urine discoloration;
- the appearance of blood in the urine;
- pain in the abdomen, groin or lower back;
- pain in the perineum;
- pain or discomfort in the penis and testicles;
- pain on ejaculation;
- increased body temperature (with acute bacterial prostatitis).
Diagnostic
According to the generally accepted classification of prostatitis NIH (US National Institutes of Health), there are four categories of diseases, traditionally designated by Roman numerals:
- I - acute bacterial prostatitis;
- II - chronic bacterial prostatitis;
- III - chronic abacterial prostatitis / chronic pelvic pain syndrome (CP / CPPS);
- IIIa - chronic prostatitis / chronic pelvic pain syndrome with signs of inflammation;
- IIIb - chronic prostatitis / chronic pelvic pain syndrome without signs of inflammation;
- IV - chronic asymptomatic prostatitis (asymptomatic).
Despite the widespread prevalence of prostatitis, acute bacterial prostatitis is not common - 5% of all cases of the disease. But its diagnosis is quite simple, because the picture of the disease is most often pronounced: a man complains of frequent and painful urination, pain in the uterus and perineum. A rise in body temperature is characteristic, and often at high values - below 39 ° C.
The diagnosis of acute bacterial prostatitis involves a digital rectal examination (rectal exam), which involves feeling (palpating) the prostate with the index finger through the anus (rectum).
The digital rectal examination (DRE) is an important diagnostic manipulation if a pathology of the prostate is suspected. Therefore, men are advised not to refuse to drive it.
In acute bacterial prostatitis, the prostate on palpation is very painful, edematous, most often enlarged. Ultrasound can show not only an increase in the size of the prostate, but also foci of purulent fusion of prostate tissue (abscess) - but this happens rarely and, as a rule, is the consequence of an ongoing process.
Laboratory diagnosis first of all includes a general urine test, in which an increase in the number of leukocytes is noted. Bacteriological urine culture is recommended. Based on the results of the analysis, it is possible to determine the presence of bacteria and their sensitivity to the antibiotic, and thus adjust the prescribed antibiotic therapy. A general blood test is also done to assess the general condition of the body and its response to the inflammatory process.
Taking prostatic secretions for the diagnosis of acute prostatitis is contraindicated due to the increased risk of a potentially fatal disease: bacteremia and sepsis. The determination of the oncomarker (PSA) and its fractions is also not recommended - due to the low information content and data distortion in the context of inflammation.
Treatment of prostatitis
Antibiotic therapy is the basic treatment for patients with prostatitis of all categories.
Alpha blockers are also an effective group of drugs. Due to their action, the tone of the smooth muscles of the prostate, neck of the bladder and prostatic part of the urethra decreases, thereby improving urination and reducing the possibility of urine entering the prostate (intraprostatic refluxurine), which is one of the causes of prostatitis. The most effective and popular drugs are tamsulosin and silodosin. They are also widely used to improve urination in patients with prostatic hyperplasia.
It is possible to use anti-inflammatory drugs (Diclofenac), which effectively reduce pain and discomfort during urination, reduce swelling of the prostate, and also contribute to some improvement in the quality of urination.
Acute bacterial prostatitis is often a reason for hospitalization in a hospital, where antibiotic therapy in the form of intravenous injections is prescribed. After stabilization of the patient's condition, the patient continues to receive antibiotics in the form of tablets for 15 days or more in order to prevent the transition from acute prostatitis to chronic bacterial prostatitis.
According to statistics, 10% of patients with acute prostatitis develop chronic bacterial prostatitis. Another 10% of patients will develop chronic pelvic pain syndrome (chronic prostatitis IIIb) in the future.
How is the treatment of prostatitis in the clinic
Urologists treat prostatitis and other diseases of the genitourinary system, based on international clinical guidelines. This means that they not only use their professional knowledge, but are also guided by scientifically proven and accepted worldwide diagnostic and therapy methods.
Our doctors do not prescribe ineffective drugs and "just in case" tests, do not cure diseases that do not exist. When making a diagnosis, urologists rely on the data obtained during the examination of the patient, the clinical picture, data from laboratory and instrumental studies. If surgical treatment is required, surgical operation is carried out on the territory of the clinic.

























